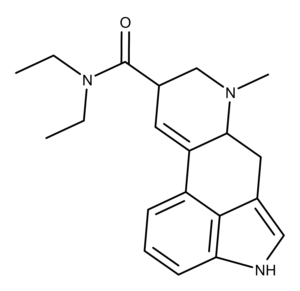
LSD (lysergic acid diethylamide) is an iconic psychedelic drug popularized by Timothy Leary and others as part of the 1960s counterculture movement. LSD is a synthetic psychedelic compound, unlike naturally-occurring psychedelic compounds like psilocybin and psilocin.
The Chemistry of LSD
In 1938, Swiss chemist Albert Hofmann (1906-2008) became the first person to synthesize and ingest LSD.1 It was the twenty-fifth derivative he synthesized from the ergot fungus, hence its more proper name, LSD-25.
LSD is the most potent psychedelic agent in humans.2 It belongs to the ergoline family of psychedelic compounds, also called rigidified tryptamines. LSD has intriguing chemistry in that its chemical structure can only be manipulated in a few ways, and any of those modifications will “attenuate its activity by about an order of magnitude.” Researchers have not spent much time on trying to modify (improve on) LSD “Because of its structural complexity and tedious approaches to its total synthesis.”
Studies have shown that the 9,10-double bond in LSD is essential for its psychedelic effect.3,4 Additional research indicates that its high potency (in vivo) depends on the N,N-diethylamide moiety.5
The Pharmacology of LSD
A 2008 review article by Torsten Passie et al. summarizes the psychological, acute neurocognitive, and somatic effects of LSD.6 The psychological effects of a moderate oral dose of LSD (75-150 µg) include euphoria, enhanced capacity for introspection, perceptual changes such as illusions and synesthesia, distorted sense of time, and changes in body image and ego function. LSD impairs coordination and reaction time and decreases performance on tests of concentration and attention. The physical effects of LSD include dilation of the pupils and low to moderate increases in heart rate and blood pressure, salivation, and sweating.
The Pharmacokinetics of LSD
The onset of effects from a 1 µg/kg oral dose of LSD is about 30-45 minutes, and only a few minutes for an intravenous dose of 16 µg/kg.7 Peak effects occur 1-3 hours after oral administration. The duration of effects is dose-dependent: 6-8 hours at 1 µg/kg and up to 10-12 hours at 16 µg/kg. LSD is quickly distributed from the blood plasma into the body tissues and is ultimately metabolized in the liver.
A 2016 study using 16 healthy subjects (8 female and 8 male) found 1% of orally-administered LSD (200 µg) was eliminated in the urine as LSD.8 Within 24 hours, 13% was eliminated as 2-oxo-3-hydroxy-lysergic acid diethylamide. There was no difference in the pharmacokinetic data based on sex. The subjective effects of the participants and their physiological responses to LSD lasted up to 12 hours. The effects were closely associated with the plasma concentration of LSD over time, and no acute tolerance was seen.
The Pharmacodynamics of LSD
In 1998, Vollenweider et al. used psilocybin and receptor antagonists to demonstrate the involvement of the serotonin 5-HT2A receptor (5-HT2AR) in the psychedelic experience.9 In the same paper, the researchers reported that the dopamine antagonist and antipsychotic drug haloperidol enhanced the effect of psilocybin on 5-HT2AR. Since that time, research has found that that the hallucinogenic response requires 5-HT2AR forming a complex with the G protein-coupled receptor protein mGluR2.10 In 2018, Preller et al. further confirmed the involvement of 5-HT2A in the effects of LSD using cortical gene expression maps.11
In 2017, researchers solved the crystal structure of LSD bound to the 5-HT2BR.12 This study made several significant observations about how LSD binds to the receptor and the subsequent cellular signaling it elicits. The 5-HT2AR and 5-HT2BR have enough similarities in their binding of LSD and other compounds that researchers consider 5-HT2BR an excellent model system for 5-HT2AR.12 Therefore, what is learned by studying 5-HT2BR can shed light on the functioning of 5-HT2AR.
The crystal structure showed the researchers that LSD has an unexpected configuration when bound to 5-HT2BR.12 Specifically, the receptor undergoes conformational rearrangements that are needed to bind LSD’s diethylamide moiety. These rearrangements included changes in the sidechain conformations of several amino acid residues that known to be important for binding LSD. Further, the researchers say, “These structural rearrangements suggested to us that LSD’s positioning in the binding pocket—mediated by the amide substituent–might be important for its signaling.”
This study also found that LSD dissociates from 5-HT2BR and 5-HT2AR exceptionally slowly.12 The researchers think this may be due to a “lid” that they saw formed in one of the receptor’s extracellular loops located at the entrance to the binding pocket. This lid, they theorize, hinders LSD’s ability to escape from the binding site, prolonging its effect. When they modified the receptor with a mutation that increased the mobility of the lid, this greatly accelerated the binding kinetics of LSD, meaning it didn’t stay bound as long.
Another important finding from this study has to do with how LSD’s binding changed a receptor signaling pathway. Research data now show that LSD activates signaling proteins called ß-arrestins.13 These proteins are, in part, responsible for “turning off” a response by blocking the signaling pathways of GPCRs. Using the same receptor model modified with the mutation as described above, the data revealed that the greater mobility of the receptor lid caused dampening the ß-arrestin signaling brought on by the binding of LSD.12 Also, the data showed that the slow binding kinetics of LSD is essential for these signaling kinetics to work.
LSD also has significant affinity and agonist activity at dopamine receptors, particularly D2R.14,15 This is an interesting phenomenon given dopaminergic systems are not known to be involved in eliciting the effects of the classic serotonin hallucinogens. However, a recent study indicates that when LSD binds to 5-HT2AR, it causes allosteric modulation of D2R.16 This modulation leads to the creation of a D2-5-HT2A receptor complex, which enhances recognition and signaling between the receptors. This mechanism may contribute to the hallucinogenic effects of LSD and help explain its effects at very low doses.
The Applications and Potential of LSD
Although the US Drug Enforcement Agency (DEA) still has LSD on Schedule I “with no currently accepted medical use and a high potential for abuse,” research entities with sufficient resources have been able to study its use to treat conditions such as depression, anxiety, alcoholism, and cluster headaches.
The first study using LSD to treat depression was undertaken in 1952.17 In summarizing the study results, the authors stated, “Improvement obtained during the course of LSD therapy was not greater than that obtained without its use in comparable cases. However, LSD affords therapeutically valuable insights into unconscious processes by the medium of the hallucinations it produces.” Since that time, researchers have had promising results using LSD-assisted therapy in clinical trials for treating the anxiety and depression associated with life-threatening diseases.18
The use of LSD to treat alcoholism goes back to the work of British scientist and researcher Humphry Osmond which began in 1952.19 Dr. Osmond realized that LSD produced symptoms similar to delirium tremens and alcoholics often attributed their ability to quit drinking to the horrific experience they have withdrawal and not wanting to go through it again. Osmond set out to dose the alcoholic patients with LSD, hoping to scare them into changing their ways. He was astonished when the patients had interesting rather than frightening experiences on the drug. Also, 40-45% of those treated with LSD had stayed sober a year after their treatment.
In 2012, Krebs and Johansen published a meta-analysis of six randomized controlled trials using LSD to treat alcoholism.20 Their analysis of the pooled data revealed that a single dose of LSD “had a significant beneficial effect on alcohol misuse at the first reported follow-up assessment, which ranged from 1 to 12 months after discharge from each treatment program.” The beneficial effects were also seen at 2-3 and six months follow up and waned to not statistically significant after 12 months.
Sewell et al. analyzed survey data on the effects of self-medication with LSD or psilocybin on cluster headaches in 53 people.21 Both compounds showed promising results, including the observation that a single dose of LSD induced remission periods of cluster headaches. The authors acknowledge that additional research is needed because of several limitations of their study. These include recall bias, selection bias, the possibility of a placebo response because the patients were not blind to their treatment.
The practice of microdosing LSD and other psychedelics for medical reasons and to enhance creativity, decision making, and personal fulfillment has become popular recently. However, based on a recent study published by Imperial College London, it is unknown at this point if microdosing works (and exactly how to define a microdose).22 The authors concluded from their analysis of experience reports and other information that there is insufficient scientific evidence to conclude that microdosing works. Aside from all the uncontrolled variables such as potency, dosage, etc., another big issue is that the majority of microdosing reports are anecdotal and tend to focus only on positive experiences.
Researchers may have only scratched the surface in revealing the applications and potential of LSD. Additional research would improve understanding of its mechanisms of action and perhaps how it can be used in conjunction (entourage effect) with other compounds to treat conditions and improve existing therapies.
Dose Data
| Dose (mg/kg) | Administration | Species | Ref. | |
|---|---|---|---|---|
| LD50 | 46 | Intravenous | Mouse | 23 |
| LD50 | 16 | Intravenous | Rat | 23 |
| LD50 | 0.3 | Intravenous | Rabbit | 24 |
| TDLO | 0.007 | Oral | Human | 25 |
Receptor Binding Affinity Data
| Receptor | Ki (nM) | Species | Note | Ref. |
|---|---|---|---|---|
| 5-HT1A | 1.1 | Human | 26 | |
| 5-HT2A | 0.75 | Human | 27 | |
| 5-HT2B | 3.71 | Human | 28 | |
| 5-HT2C | 1.09 | Human | 27 | |
| D1 | 180 | Rat | 26 | |
| D2 | 120 | Rat | 26 | |
| D3 | 27 | Rat | 26 | |
| D4 | 56 | Rat | 26 | |
| D5 | 340 | Rat | 26 |