Part 1 of this article series focused on the broad repertoire of peripheral tissues that express psychedelic target receptors throughout the body. However, given the uniqueness of each structure within the human body, the systems where psychedelics could exert effects call for specific discussions.
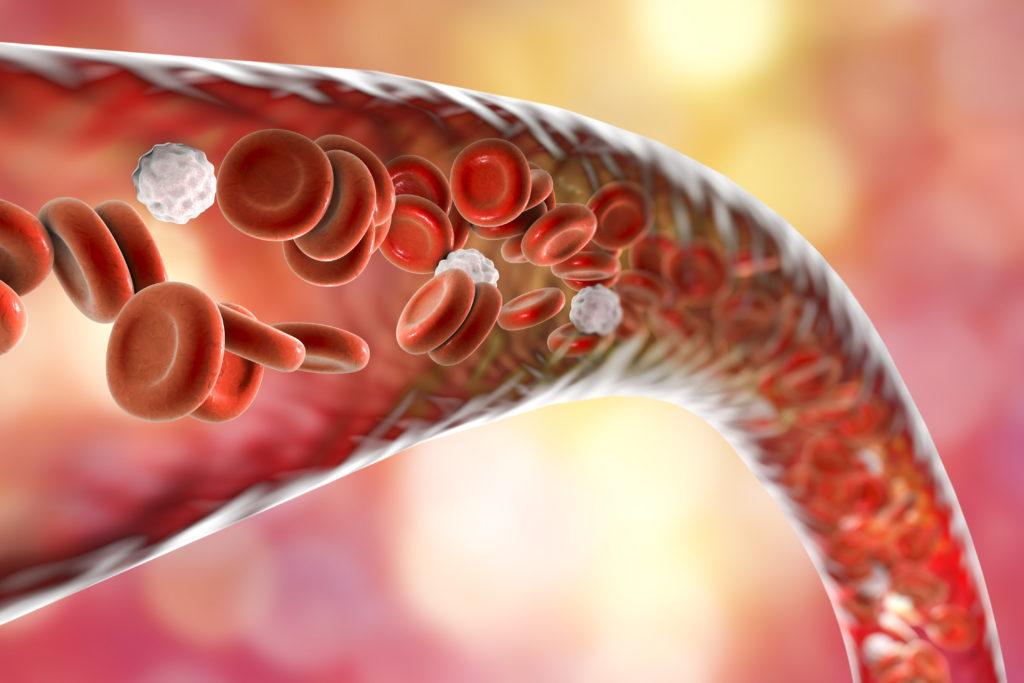
A couple of minutes after psychedelic intake, many organs and aspects of behavior are influenced by these powerful molecules. However, no matter the destination, the blood is a road they must travel. Indeed, research indicates that the amount of some classic psychedelics like LSD and psilocin reaches its maximal concentration in plasma within hours after oral ingestion and remains there long enough to interact with blood components.1,2
This means that the blood, the 5 liters of highly adaptive omnipresent circulating fluid-tissue in the human body, is flooded with psychedelics. As the blood is responsible for delivering oxygen and nutrients to all living cells in the body and collecting their waste products, it also makes these external substances available everywhere once they are in plasma. However, even though it’s often seen as an intermediate route for most scientific questions, the blood is filled with cells and structures expressing psychedelic target receptors.3 The immune cells, which represent a large part of blood components, express almost all serotonin receptors, therefore, they are responders to serotonin agonists such as classic psychedelics.
Can the Immune Cell Army Win Fights by Tripping?
The first line of defense of the immune system is composed of innate immune cells such as granulocytes- namely basophils, eosinophils, and neutrophils.4 Whereas basophils and eosinophils play important roles for host defense against parasites and mediate allergic reactions, neutrophils are the most numerous innate cells patrolling for problems by circulating in the bloodstream. Not much is known about the effects of psychedelics on innate immune cells. However, recent studies have started to describe that selective activation of the 5-HT2A receptor prevents eosinophil recruitment in conditions such as asthma, paving the road to an exciting area for future research.5
Blood monocytes are key players of immune function and develop into macrophages and dendritic cells.4 Macrophages patrol and respond to problems by their astonishing ability to ingest and degrade infiltrating pathogens and damaged fragments of host tissues. On the other hand, dendritic cells are the professional and most sophisticated antigen-presenting cells in the system. They process large molecules derived from pathogens, damaged host cells, and allergens into easily decipherable fragments that are recognized by lymphocytes.4 The activation of serotonin receptors 5-HT1 and 5-HT7 were demonstrated to regulate the differentiation of monocytes into active dendritic cells with a less reactive profile, suggesting a regulatory role in the inflammatory process mediated by these cells.6 Interestingly, both subtypes of receptors are high-affinity targets for psychedelics such as LSD. 7
The immune cells communicate either by cell-to-cell contacts or through molecules called cytokines.4 These secreted messengers allow the immune cells to talk to each other, orchestrating the immune function. The psychedelics N,N-DMT, and 5-MeO-DMT were demonstrated to inhibit the production of pro-inflammatory cytokines while increasing the secretion of anti-inflammatory cytokines by monocyte-derived dendritic cells through sigma-1 receptor signaling.8 Via this pathway, the communication to T lymphocytes is also inhibited, limiting the immune response cascade. Moreover, the activation of 5-HT2A receptors was also shown to diminish the release of pro-inflammatory cytokines.9,10 The extraordinarily potent anti-inflammatory effect of 5-HT2A activation in vascular tissue was demonstrated to prevent the development of atherosclerosis, a human disease affecting blood vasculature with a strong inflammatory component on its pathogenesis.11
Organs involved in lymphocytes’ development and function, such as the spleen and thymus, express 6 out of 13 serotonin receptors subtypes,12 suggesting that these organs could be affected by psychedelics. The number of natural killer cells, a subpopulation of lymphocytes important for antiviral and anticancer mechanisms, is increased after ayahuasca intake and its function was demonstrated to be enhanced after low doses of LSD.13-15 Although the immunomodulatory effect of LSD remains elusive, early studies have already suggested that this molecule interferes with antibody biosynthesis in type B lymphocytes.16
By the end of the 1990s, even the psychedelic-induced mystical experience per se was proposed to boost the immune system.17 Regrettably, nothing has been investigated about this hypothesis until now. Discoveries on this topic would be groundbreaking by adding valuable insights to the ongoing debate on whether or not the subjective experience is necessary for the therapeutic effects of psychedelics – in this case, for immune benefits. Moreover, this could broaden the comprehensive link between the whole-body effects of psychedelic compounds and the perceived well-being regarding the subjective experience.
Psychedelics May Bring Fresh Blood to the Body
A shared feature of both immune cells, red blood cells, and even platelets is that they develop in the red bone marrow in a process called hematopoiesis. The formation of red blood cells is impaired in the absence of serotonin signaling in peripheral tissues, suggesting a role for serotonin receptors in the bone marrow.18 Actually, stimulation by serotonin also increases the survival of red blood cells,19 those responsible for delivering oxygen to all organs. This means that when psychedelics bind to these receptors, they could optimize the oxygen delivery to human organs by both promoting formation and maintenance of these cells. This effect could be one of the mechanisms behind a putative overall increased body function during psychedelic experiences.
When something goes wrong and damage occurs to the walls of blood vessels, the activation of serotonin receptors is one of the signals that control platelet activation to allow repair of the vessel injury.20 Even the cells lining the walls of blood vessels themselves are capable of responding to serotonin and, presumably, to psychedelics.21 In fact, at the wound site of a blood vessels’ wall, the serotonin signaling acts as a vasoconstrictor to help contain unnecessary bleeding.20 When refreshing blood cells is not sufficient and the need is for new blood vessels, signaling through serotonin receptors stimulates the formation of both vascular lining and muscular cells through 5-HT2B receptors.22,23 In addition, binding to 5-HT1B receptors was indeed shown to induce the growth of brand new blood vessels from the existing vasculature.23,24
Activation of serotonin receptors also enhances the proliferation and survival of megakaryocytes in the red bone marrow, the cells that give rise to platelets, and later, stimulates the platelet formation.25 Platelets are small cell fragments responsible for forming clots and thus stopping bleeding within the vascular system. As occurs with serotonin binding, it is likely that psychedelics, while in the blood, activate the 5-HT2A receptor on the surface of platelets stimulating their activation.26,27
However, the outcomes of serotonin receptor activation in platelets are debatable regarding cardiovascular function.28 In Part 3 of this series, this topic and research on heart function under psychedelics will be further explored.

Can’t wait to see see more research conducted in this area!
Very interesting article, I am looking forward to part 3!
Thanks, Will! Part 3 about the heart is on its way! Many interesting scientific data to review on this specific organ! I hope you all like it!
Where is part 3 on the heart ? It’s been almost a year since this article ?
Hello Mike! It took a while, but now is available at https://psychedelicreview.com/whole-body-effects-of-psychedelics-part-3-the-heart/!