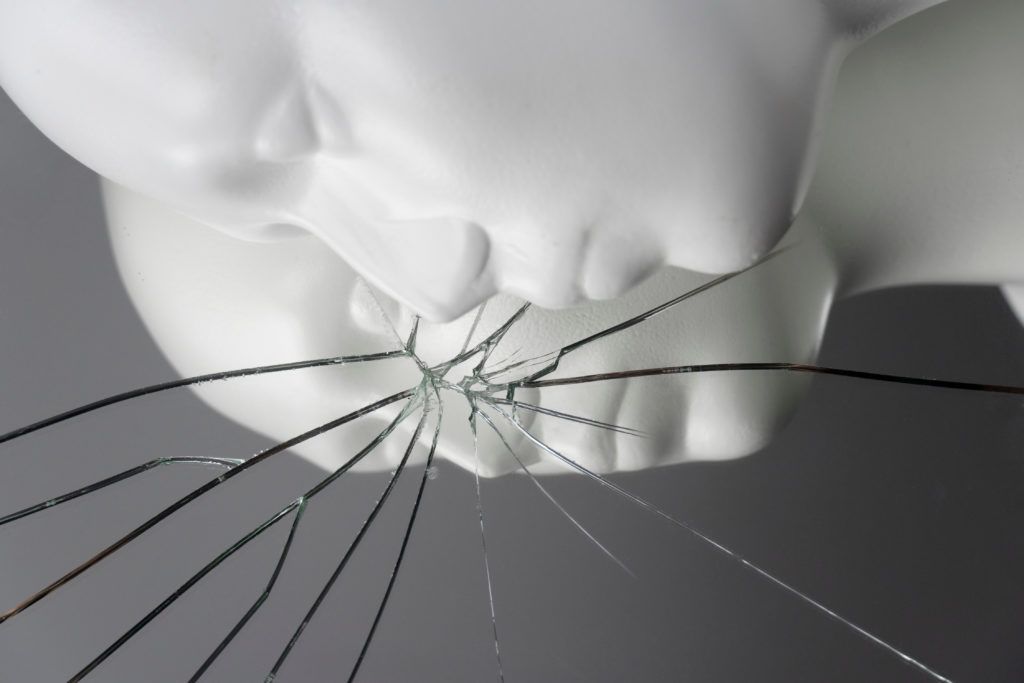
Theories of how psychedelics work in the brain are still evolving, but one of the best-supported ideas right now is the REBUS (Relaxed Beliefs Under Psychedelics) theory: psychedelics relax prior beliefs and thought patterns to make room for new, healthier ones.1 In depression, for example, they can break patterns of negative thoughts about oneself or the world at large. At the neurobiological level, this may correspond to opening a window of neuroplasticity during which there is an increased capacity for positive change.
REBUS is not only attractive for what it explains, but also for what it implies. How many other psychological disorders are characterized by persistent, maladaptive beliefs? Is there one that is not? Psychedelic research so far has largely focused on mood disorders, PTSD, and addiction, but there may be potential for other “disorders of rigidity” as well. And though psychedelics are certainly not going to fix every psychological issue, scientists are still feeling out their limits.
Borderline Personality Disorder
One candidate for clinical research is borderline personality disorder (BPD), which affects about 1-2% of the population and is characterized by extreme instability in various aspects of patients’ lives.2 Patients struggle with impulse control and unstable relationships, and their emotional lives and self-image are also highly volatile.2 BPD is a severe condition that may cause people to harm themselves or self-medicate to deal with their multifaceted emotional pain. About 10% of patients with BPD commit suicide. As far as treatment, it’s a familiar story: some therapies help some of the time, but many patients struggle chronically.5
A recent paper makes the case that psychedelics could help where other treatments fail. At first glance, psychedelics would not seem to be good weapons against a disorder characterized by instability. After all, the psychedelic state itself is highly unstable, causing people to switch rapidly between intense emotions and hallucinatory states.6 Perhaps they would just make things worse. But Richard Zeifman and Anne Wagner, both specialists in clinical psychology, say not to judge too quickly: Psychedelic therapy may be able to specifically target some of BPD’s hallmark symptoms.5 At least, they argue, it’s worth a careful shot.
Psychedelics for BPD: Four Symptoms of Interest
No direct clinical data exists on psychedelic therapy for BPD. However, many symptoms of BPD are not unique to that disorder, and previous studies have shown that psychedelics may improve some of these symptoms. For example, patients from a study on alcohol use disorder reported more control over their own behavior after psilocybin-assisted therapy.5 Similar findings exist for healthy subjects, who show reduced impulsivity and aggression after using psychedelics. Many BPD patients struggle with exactly these problems.
As with behavior, BPD patients also struggle to regulate their emotions. They experience more unpleasant emotions, such as rage, loneliness, or shame, and they are worse at coping with them.5 Psychedelics have been shown to help with emotional dysregulation, including in people who are high in BPD-like traits. Depression and anxiety, which are characterized by specific deficits in emotional regulation, respond particularly well to psychedelics.3 To the extent that psychedelics improve people’s ability to regulate their own emotions – rather than being controlled by emotion – they may help BPD patients the same way they help those with mood disorders. Additionally, psychedelics synergize nicely with mindfulness practice, which is already an effective tool to help patients understand and manage turbulent feelings.5
Perhaps as a consequence of dysregulated behavior and emotions, people with BPD also struggle with maintaining healthy relationships. They may find it hard to trust or empathize with others and can be highly sensitive to exclusion and rejection.5 Psychedelics, in particular psilocybin and MDMA, have been associated with improvements in relationships and enhanced feelings of empathy, trust, and closeness to others. They may also reduce sensitivity to rejection and others’ negative facial expressions, and therefore emotional reactivity. Given that social problems are some of the hardest BPD symptoms to treat, drugs that make relationships easier would be valuable therapeutic tools.
Lastly, BPD is characterized by instability in someone’s sense of who they are – their identity. People may see themselves very negatively and have difficulty showing themselves compassion, or they may have an incoherent and confused sense of identity.5 Psychedelics may particularly help with the first problem: they consistently encourage patients and healthy people alike to be kinder to themselves and see their own positive qualities.
Slow and Safe Wins the Race
Though psychedelics could improve some symptoms of BPD, this is all speculative. Therapists are highly cautious about including BPD patients in psychedelic studies, mainly due to concerns that they could make an unstable condition worse.6 How might clinicians figure out whether psychedelics will really help, without exposing patients to unnecessary harm?
One conceivable avenue could be that of compassionate use exemptions. In Switzerland, for example, approved physicians may request permission to treat patients with psychedelic therapy based on their professional judgment of how an individual patient will respond. A few patients with BPD have been legally treated in this way and seemed to respond well, though they have not been systematically analyzed.4
Importantly, many of these patients had other disorders as well. Accepting patients with specific comorbidities for clinical trials would allow researchers to offer patients a likely benefit from psychedelic therapy, while also investigating whether BPD symptoms improve. Indeed, one study of ayahuasca therapy for treatment-resistant depression has included several participants with comorbid BPD, all of whom showed an improvement in depressive symptoms without any worrying adverse effects.7 That study did not investigate BPD symptoms specifically, but future ones could.
Either way, clinicians considering psychedelic therapy for BPD agree that safety precautions are even more important than usual.6 Due to BPD’s unstable nature, it may take a particularly skilled therapist to work with these patients. Building an effective therapeutic alliance, which is essential for safe psychedelic therapy, could be more challenging than usual. Therapists would have to be able to carefully prepare their patients, set their expectations, and convince them to commit to the difficult work inherent in psychedelic therapy. If they can do that, a cautious exploration of psychedelics for BPD might take place.
Ketamine, which shares some mechanisms of action with classic psychedelics, is currently being investigated for treating suicidality in BPD in a Phase 2 clinical trial at Yale. For more information, visit clinicaltrials.gov.
As someone diagnosed with BPD, and who has some experience with psychedelics, I can say it’s a bit of a mixed bag. I find a full dose of mushrooms is too intense for me to navigate and I lose it hard. (Although I may also be Autistic… it’s difficult to get a diagnosis as an adult). Microdosing, however, has gotten me through some horrible experiences without quite as much residual trauma as I had expected. I’ve tried MDMA a few times in varying doses, and have had an awful time every time. Never enjoyed it even a little. Microdosing LSD… Read more »
What would you say worked best for you? If you could rate each substance on a 1-5 or 1-10 scale. Specifically k v.s. mushrooms
Is there anywhere to participate in a clinical trial for BPD using psychedelics?
Looking for a clinical trial for BPD using psychedelics
It looks like the university of Chicago has been conducting research on this particular topic. If you google search psychedelics and bpd , you will come across a scholarly article and their contact info.
I was diagnosed with BPD when I was 18, I had struggled with depression and suicide ideation for years and was very self destructive. As time went on I was trying to help myself with my symptoms and sense of self and accept myself and my past with varying degrees of success. In 2016 I stumbled upon lectures by a psychologist who then introduced me to some core ideas of Carl Jung and something just clicked for me, I went down an amazing rabbit hole of self discovery and taking my recovery very seriously to a degree I hadn’t previously.… Read more »
Thanks for sharing your experience. Did you microdose with mushrooms, or do occasional larger doses?
Wow! What a beautiful story of healing and the deeper discovery of self. I hear you when you say how psychedelics were part of the journey. May you continue to grow/
I’m a 34 yo old male not diagnosed, but pretty sure i have bpd as i struggle with almost every point listed on the dsm beside suicidal attempts (temper tantrums, emptiness, depersonalization, paranoia, fear of abandonement, impulsivity in sexual behavior and spending, and multi drug use which i tend to see as psychological self harm). I’m fairly experienced with psychedelics, mindfulness and i’m now seeing a swiss jungian analyst which i find helpful as another user said. I think psychedelics and individuation work helps, provided the surrounding environment is supportive. The added neuroplasticity could help but also create new negative… Read more »
Hi, just thought id share my thoughts incase anyone wants to hear. As a person who hasnt suffered with bpd, but has grew quite close to someone who has, i feel all sympathy to anyone who has suffered, or more than likely is suffering. I have cried several times just imagining the pain one has to endear. It crushes people. It eats upon their lives as they have to endure it with no remorse. I would do anything to help my friend. I just want to see her happy and joyful all the time rather than sometimes. I just want… Read more »
I have struggled with mental health my entire life. I was diagnosed with bipolar ADHD, OCD, severe depression and many more mental health issues at a very young age. I have been in and out patients facility’s my entire life. In 2017 I had a mental breakdown. I was diagnosed with BPD On top of agoraphobia, ADHD, OCD and severe depression With suicidal thoughts. I had tried every medication clinic trial with no relief in sight. I couldn’t live like this anymore. I was introduced to psilocybin After trying lower doses at no success, I decided to try a heroic… Read more »